PK/PD Modeling and Simulation
How quantitative models turn data into decisions that de-risk development and win regulators’ confidence
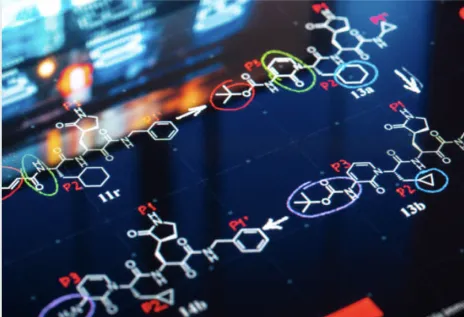
Pharmacokinetic/pharmacodynamic (PK/PD) modeling and simulation are now indispensable tools across drug discovery and development. For data-centric consultancies, these methods provide a rigorous, reproducible way to predict human pharmacology, define safe and effective doses, and optimize trial designs — all without performing wet-lab experiments. This article explains what modern PK/PD modeling delivers, how mechanistic and empirical approaches differ, and how these tools are applied to accelerate development and strengthen regulatory submissions.
What PK/PD modeling does — a quick primer
PK modeling describes how the body handles a drug (absorption, distribution, metabolism, elimination). PD modeling characterizes the time course of the drug’s biological effect. Linking PK and PD quantitatively allows teams to predict how different doses and regimens will influence target engagement, biomarker responses and clinical outcomes. Modeling therefore bridges concentration to effect and converts sparse data into actionable predictions.
Mechanistic versus empirical models
Two broad modeling philosophies are used in practice:
- Empirical models (non-compartmental analyses, simple compartmental or population PK) rely heavily on observed data to summarize exposure and variability. They are fast, robust, and sufficient for many regulatory endpoints like bioequivalence or basic dose-proportionality assessments.
- Mechanistic models encode biological processes — target binding, receptor turnover, signal transduction, tissue distribution and feedback loops — to capture causal pathways between exposure and effect. Because they separate drug-specific parameters from system-specific parameters, mechanistic models are more powerful for extrapolation (e.g., from animals to humans, or from adults to pediatrics) and for exploring novel delivery systems or complex modalities.
Both approaches are complementary: empirical models provide rigorous, data-driven descriptions; mechanistic models provide explanatory power and prediction when data are limited.
Key applications that add value
1. Target selection & lead optimization
Mechanistic PK/PD can screen virtual candidates by predicting how binding affinity, clearance or tissue distribution affect target coverage and duration. This lets teams prioritize leads with the best chance of achieving meaningful inhibition in vivo — saving time and experimental cost.
2. Translational dose projection (First-in-Human)
Models combine preclinical PK and pharmacology with human physiological parameters to simulate likely clinical exposures and support first-in-human dose selection. As clinical data accrue, models are updated to refine dose ranges for proof-of-concept studies.
3. Dose selection and exposure–response
Exposure–response analyses integrate biomarker and clinical endpoint data to identify therapeutic windows, inform dose escalation, and justify pivotal dose choices. These models underpin label claims and dosing recommendations for special populations.
4. Drug–drug interaction and special populations
PBPK (physiologically based pharmacokinetic) and population PK methods are used to quantify DDI risks and project effects in renal or hepatic impairment, pediatrics, or the elderly. Regulatory agencies increasingly accept model-based DDI assessments in place of some clinical studies when models are well-validated.
5. Formulation and delivery optimization
PBPK models can assess oral absorption risks (solubility, dissolution, permeability) and simulate the impact of formulation changes (salt form, amorphous dispersions, lipid systems) on systemic exposure — informing formulation strategy and reducing the need for repeated empirical studies.
6. Clinical trial simulation
Simulating trials with population PK/PD models lets sponsors evaluate “what-if” scenarios: sample size, dosing arms, inclusion criteria, and endpoint sensitivity. These simulations reduce trial risk and improve the probability of meaningful results.
Data, software and deliverables (data-only consulting)
High-quality, well-structured data are the prerequisite for trustworthy models. Typical inputs include plasma concentration-time data, biomarker or efficacy readouts, in vitro ADME parameters, and literature or physiological priors for system parameters. Key deliverables from a data-centric modeling engagement include:
- Protocol-aligned Model Analysis Plans (MAPs) and prospective analysis plans.
- Clean, analysis-ready datasets (SDTM/ADaM style where required) and traceable derivations.
- Non-compartmental analysis reports (NCA) with PK parameters (Cmax, Tmax, AUC, T½, CL).
- Population PK and PK/PD model code, diagnostics, and Model Analysis Reports (MARs).
- PBPK model files, scenario simulations, and sensitivity/uncertainty analyses.
- Clinical trial simulation outputs and recommended trial designs.
- Regulatory text for briefing packages, clinical overviews and submission modules.
All modeling work should be reproducible, version-controlled and accompanied by documented assumptions and uncertainty bounds so reviewers can evaluate robustness.
Workflow and good practice
A robust modeling engagement follows an iterative, transparent process:
1. Question of interest. Define the decision the model must support (dose selection, DDI waiver, pediatrics, etc.).
2. Data inventory & gap analysis. Assess available PK/PD, in-vitro and preclinical data and identify critical missing elements.
3. Model selection & MAP. Choose empirical or mechanistic approaches and pre-specify endpoints, diagnostics and acceptance criteria.
4. Model development & qualification. Build models, perform goodness-of-fit checks, cross-validation and predictive checks.
5. Simulation & decision support. Run scenario analyses for dosing, trial design, or DDI assumptions.
6. Documentation for regulators. Produce MARs, datasets, code and clear interpretive text for submissions or briefing meetings.
7. Update & iterate. Refine models as new clinical data arrive.
Regulatory context and communication
Regulators expect transparent modeling: pre-specified MAPs, clear reporting of assumptions, and sensitivity analyses. Early engagement — presenting approaches and key uncertainties in pre-IND or End-of-Phase meetings — reduces surprises and increases the chance that model-based justifications will be accepted. A well-documented model can replace or narrow clinical studies, speeding development while preserving safety.
Why work with a data-first PK/PD consultancy
Specialized consultancies focused on modeling and simulation bring deep quantitative expertise, regulatory experience, and the disciplined workflows needed to convert raw PK/PD data into defendable, decision-grade evidence. They allow sponsors to leverage model-based strategies across discovery, translational, and clinical phases while avoiding wet-lab complexity.
Conclusion
PK/PD modeling and simulation convert fragmented concentration and biomarker data into a coherent, predictive framework for decision-making. Whether empirically driven or mechanism-based, these models reduce uncertainty, optimize dosing, inform trial design and strengthen regulatory interactions. For sponsors seeking efficient, evidence-based paths to approval, disciplined modeling and simulation — coupled with rigorous data management and clear documentation — are essential.
At XP Pharma Consulting, we have several decades of experience in clinical pharmacology and can guide you from early stage to late stage drug development clinical pharmacology regulatory process. Contact us to schedule a call with an expert.

Comments are closed here.